Did you recently turn 65? If so, you may wonder: does Medicare cover CPAP machines and supplies? The short answer is yes! Medicare typically covers up to 80% of the cost of your CPAP machines and other durable medical equipment after you’ve met the Part B deductible. But what does that mean, and how do you qualify for coverage? Below, we’ll break down Medicare guidelines, qualifying requirements, replacement schedules, and how Aeroflow Sleep can help you navigate the process.
In This Article:
Does Medicare Cover CPAP Machines?
Does Medicare Cover Sleep Apnea Testing?
How Long Will Medicare Pay for CPAP Supplies?
Aeroflow Sleep Is Here To Help Medicare Patients
CPAP Therapy Through Insurance:
Aeroflow Sleep is in-network with most primary insurance companies and is accreditted by Medicare and Medicaid. Complete our Qualify Through Insurance Form, and we will automatically check to see if your plan covers CPAP supplies; including a machine, mask, and accessories. ***Must have a sleep study to qualify.***
You will also receive the care and attention every sleep apnea patient deserves; one-on-one clinical support in-home or via telehealth, a dedicated Sleep Specialist you can contact during business hours, and a user-friendly online portal with tailored replacement schedule, important updates and notifications, and educational resources.
Let us take the headache out of healthcare. Join the Aeroflow Sleep family today! It only takes 5-7 minutes to get started.
Does Medicare Cover CPAP Machines?
Medicare has two main parts that cover different types of care: Part A and Part B. While Medicare Part A handles inpatient care, hospice, and skilled nursing, Medicare Part B works like standard health insurance, covering outpatient visits, routine screenings, prescription treatments, and equipment like CPAP machines.
Coverage for Medicare and CPAP supplies falls under Part B and includes everything from machines to accessories like tubing, full-face masks, and humidifier chambers—once you’ve met the deductible.
Here’s how it works:
- The deductible is the amount you pay before Medicare begins covering costs.
- Once met, Medicare pays 80%, and you are responsible for the remaining 20% of your CPAP machine and supplies.
Your clinician and Durable Medical Equipment supplier (or DME supplier) must both be approved by Medicare. Luckily, Aeroflow Sleep is!
If you need a clinician, we can refer you to Michelle Worley, our Director of Clinical Operations at Aeroflow Sleep and a Registered Nurse. She and other members of the Aeroflow Sleep team are available to assist you.
As your DME supplier, we can also navigate your machine rental. Medicare rents CPAP equipment for 13 months of continuous use to help keep overall costs lower. This also ensures they’re only paying for items that are being used, and it is only when you have successfully met the 90-day compliance requirements and surpassed 13 months of continuous use that we can transfer ownership to you.
Does Medicare Cover Sleep Apnea Testing?
Yes, Medicare Part B typically covers sleep apnea testing if deemed medically necessary. This includes both at-home sleep tests and in-lab sleep studies, provided they are ordered by your doctor and conducted by a Medicare-approved provider.
For Medicare to approve coverage, your doctor must document your symptoms, such as excessive daytime sleepiness, loud snoring, or observed pauses in breathing during sleep. Once approved, the test results will determine your eligibility for CPAP therapy.
Qualifying For A CPAP Through Medicare
Qualifying for a CPAP machine through Medicare is easy with Aeroflow Sleep! Simply follow these 3 simple steps:
1. Determine Your Eligibility
To qualify for Medicare, you need to meet certain requirements:
-
Be 65 or older and either a U.S. citizen or a permanent resident for at least five consecutive years.
-
You may also qualify earlier if you have a disability or a condition like End Stage Renal Disease (ESRD).
If you’re already receiving Social Security or Railroad Retirement Board benefits, you’re likely automatically enrolled in Medicare Part A and B. If not, you’ll need to enroll during your Initial Enrollment Period (IEP), which begins three months before your 65th birthday and ends three months after.
2. Get a Sleep Test and Prescription For a CPAP
Medicare requires a diagnosis of sleep apnea from an approved clinician to cover CPAP therapy. Your doctor can prescribe one of two tests:
- At-Home Sleep Test: Wear a small device overnight to measure your breathing and return it for evaluation by a sleep specialist.
- In-Lab Sleep Study: Spend the night in a sleep clinic for a more comprehensive test, which may be more expensive.
Your results will show your Apnea-Hypopnea Index (AHI), indicating how often you stop breathing during sleep. Medicare covers CPAP therapy if your AHI is 5 or higher and it’s deemed medically necessary.
3. Meet Medicare's CPAP Compliance Guidelines:
After receiving your CPAP machine, you’ll need to meet Medicare’s 90-day CPAP compliance guidelines:
-
Use your CPAP machine for at least 4 hours per night on 70% of nights (21 out of 30 days).
Your CPAP machine collects compliance data and shares it with your doctor, who will review your progress and verify the therapy is effective. Once Medicare CPAP compliance guidelines are satisfied, Medicare will continue covering your CPAP equipment rental for up to 13 months, after which ownership will be transferred to you.
Aeroflow Sleep offers clinical education in-home or via telehealth during setup and personalized support to help you meet compliance requirements.
How Long Will Medicare Pay for CPAP Supplies?
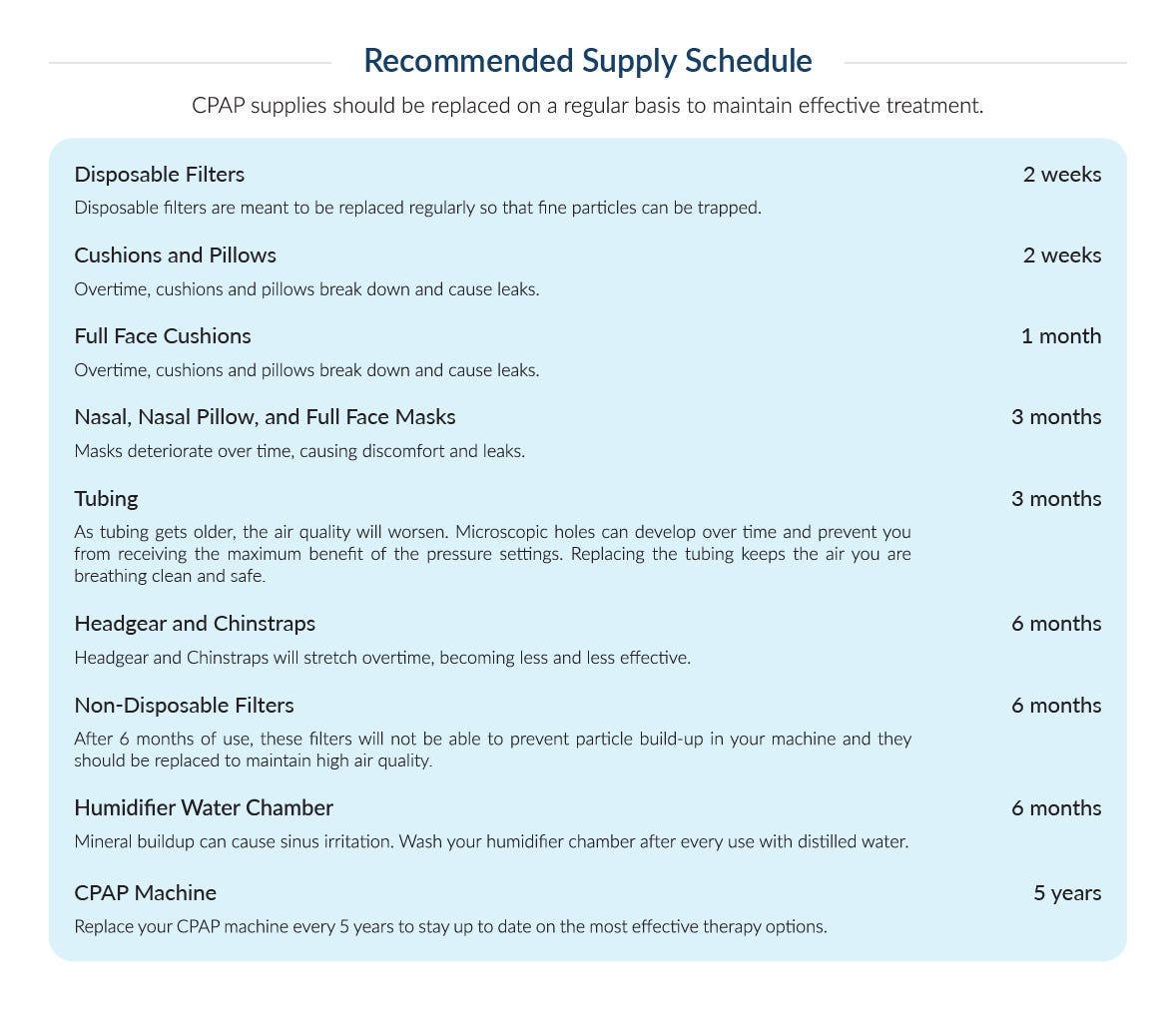
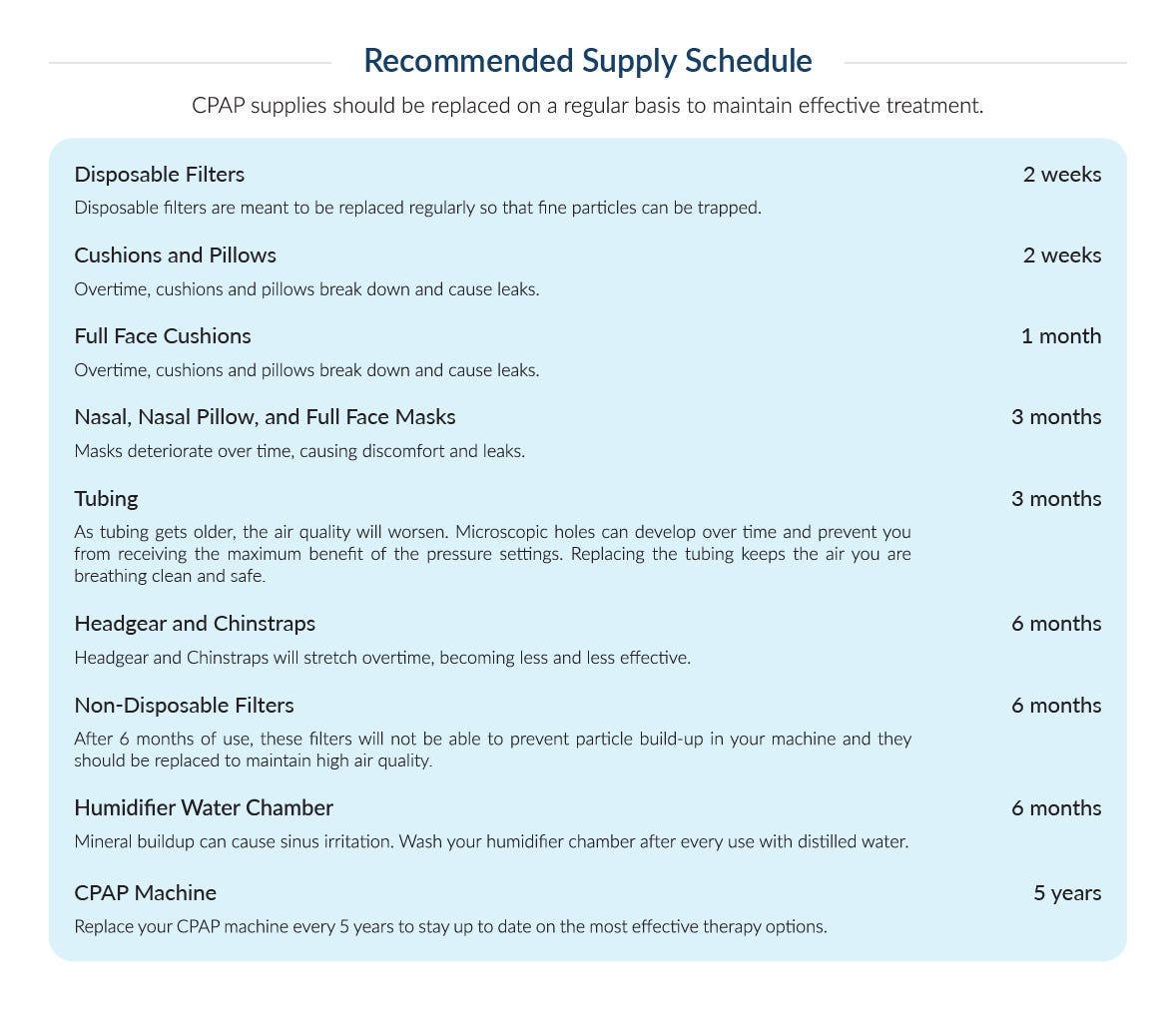
Medicare covers CPAP equipment rental for 13 months if you meet compliance guidelines. After that, ownership is transferred to you. During this period, Medicare also covers Medicare-approved CPAP supplies, such as replacement filters, tubing, and masks.
Adhering to Medicare’s replacement schedule ensures optimal therapy and hygiene. Aeroflow Sleep helps you stay on schedule by sending reminders and delivering replacement supplies to your door.
Aeroflow Sleep Is Here To Help Medicare Patients
You deserve peace of mind when it comes to your insurance, so let Aeroflow Sleep take care of it for you! As a Medicare-approved Durable Medical Equipment supplier, you will never have to wonder if your CPAP therapy is covered. Treatment options may be available at little to no cost, and we promise to find them. Start sleeping well and living better. Call (800) 480-5491 to speak with your personal sleep specialist, or sign up for your new CPAP supplies below.










