Do you qualify for Medicaid? What even is Medicaid, and how exactly does it work? And, can you get the CPAP equipment you need through Medicaid? If you’re seeking the answers to these questions or similar ones, you’re in the right place, especially since guidelines have recently changed.
IN THIS ARTICLE:
The Difference Between Medicaid & Medicare
When Does Medicaid Cover CPAP Supplies?
CPAP SUPPLIES THROUGH MEDICAID:
Aeroflow Sleep is in-network with most primary insurance companies and is accredited by Medicare and Medicaid. Complete our Qualify Through Insurance Form, and we will automatically check to see if your plan covers CPAP supplies; including a machine, mask, and accessories. ***Must have a sleep study to qualify.***
You will also receive the care and attention every sleep apnea patient deserves; one-on-one clinical support in-home or via telehealth, a dedicated Sleep Specialist you can contact during business hours, and a user-friendly online portal with a tailored replacement schedule, important updates and notifications, and educational resources.
Let us take the headache out of healthcare. Join the Aeroflow Sleep family today! It only takes 5-7 minutes to get started.
What Is Medicaid?
Medicaid is a government resource program that helps those with limited income access the medical care, equipment, and services they need. Simply put, Medicaid is insurance for people who cannot pay for healthcare. So although it’s jointly funded by the state and federal governments, it is enacted at the state level, which means what Medicaid covers varies from state to state. Each state is not required to participate, but all states have since 1982…to some degree.
In February 2023, it was announced that the United States would end its COVID-19 public health emergency (PHE) on May 11th. USA Today released, “About 15 million Americans who gained Medicaid insurance during the pandemic [were] at risk of losing coverage…as federal subsidies end.”
In April 2023, Medicaid covered 94 million low-income families and/or people with disabilities. That number is now expected to cover less than 80 million without PHE, because, as of July 31st, all states are back to independently managing the access given to its Medicaid recipients; including those with sleep apnea. So, are you still eligible for Medicaid post-pandemic…? Let’s find out!
Am I Eligible For Medicaid?
For Medicaid eligibility, you must be a United States citizen and low-income adult (with or without children) or someone who has a certain disability; such as a developmental or intellectual disability. Non-citizens who fit the same description may also be eligible if they are considered “lawfully present immigrants;” such as lawful permanent residents or green card holders.
You will most likely qualify for Medicaid if you make less than 100-200% of the federal poverty line (FLP) and are pregnant, disabled, elderly, or the parent or guardian of a child.
There is no age limit for Medicaid eligibility like there is for Medicare, but each state does set requirements based on age, as well as income, household size and role, the nature of a person’s disability, and whether or not you are pregnant. This begs the question, what is the difference between Medicaid and Medicare?
The Difference Between Medicaid & Medicare
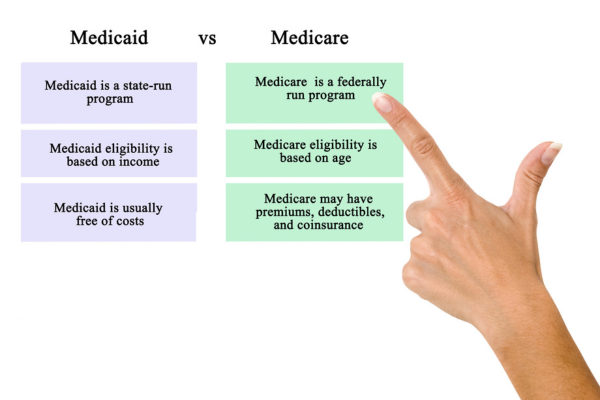
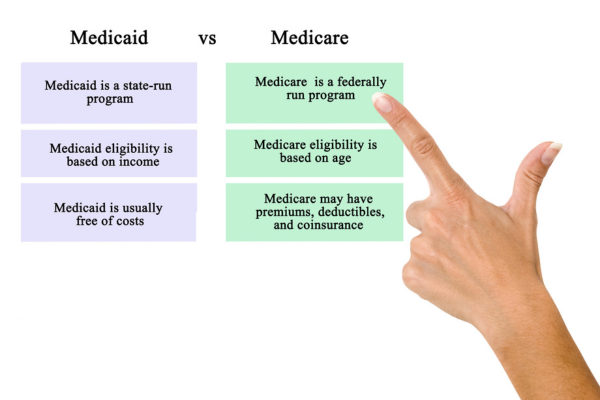
Medicaid and Medicare are not the same. They are two different programs that are operated and funded by very different portions of the government, primarily to serve different groups of people with different needs. Oh, and did we mention they’re different?
How are they different? Remember, Medicaid is available to everyone—no matter your age—as long as you meet the individual requirements set by your state. Medicaid is also funded by taxes collected from the public; it’s a need-based program. Whereas, you must be 65 or older to apply for Medicare (unless you have a separately listed disability,) and income is not a factor.
Because income is not a factor, Medicare-covered medical services may require payment. These are generally plans that offer additional coverage, of which CPAP supplies are often included; typically, 80% of the cost of CPAP supplies is covered by Medicare, and you would pay for the rest. This isn’t the same for CPAP supplies covered by Medicaid.
When Does Medicaid Cover CPAP Supplies?
It’s not a question of when Medicaid covers CPAP supplies but where. You can probably bank on Medicaid covering your CPAP machine, but masks and supplies may be another story. Rather than list which state covers which piece of CPAP equipment, Aeroflow Sleep recommends enrolling in Medicaid and contacting us to help determine your state-by-state coverage.
How Do I Apply For Medicaid To Get My CPAP Supplies?
To apply for Medicaid, you need to complete the appropriate application for your state. There’s no enrollment period, and you can apply online. Some states will even allow you to submit a paper application. With a paper application, you do not have to go to your Medicaid office. You can mail it, fax it, or (if you insist) return it to your local government office.
Be sure to have the following in front of you when completing the application:
- Birth Certificate or Driver's License: Used to verify age and citizenship
- Medical Records: Used to verify disability
- Recent Pay Stubs or Tax Returns: Used to verify income
- Properly Lease or Utility Statement: Used to verify address
- Bank Statements: Used to verify savings resources
Each state has 45 days to process your application; and 90 days if your eligibility includes a disability. And, don’t worry; if you don’t qualify, you may still be offered subsidized healthcare plans from the federal government. This is especially true for those who recently lost Medicaid coverage due to PHE ending.
Once you’ve qualified, all that’s left is to advocate for you and your sleep apnea. Aeroflow Sleep’s parent company, Aeroflow Healthcare recently launched its Government Relations Program to help ensure equitable access to care at both the state and federal levels. Ryan Bullock, COO, says, “Expanding government relations capabilities…will only enable us to continue pushing more proposed solutions to improve the lives of the individuals and families we serve,” so put your trust in us. Remember to notify Aeroflow Sleep of any changes in insurance coverage; Medicaid or otherwise. We’re here to help!
References
Rodriguez, Adrianna, and Ken Alltucker. “The COVID Public Health Emergency Is over in the US. Here’s What That Means for You.” Health, 11 May 2023, www.usatoday.com/story/news/health/2023/05/11/end-covid-public-health-emergency-explained/70182594007/.
“April 2023 Medicaid & CHIP Enrollment Data Highlights.” Medicaid & CHIP Enrollment Data, May 2023, www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html.
“What’s the Difference between Medicare and Medicaid?” Medicare and Medicaid, Aug. 2023, www.hhs.gov/answers/medicare-and-medicaid/what-is-the-difference-between-medicare-medicaid/index.html.
“Select Your State for Medicaid Eligibility or to Apply for Coverage.” Beneficiary Resources, Aug. 2023, www.medicaid.gov/about-us/beneficiary-resources/index.html#statemenu.
Staff, HME News. “AEROFLOW LAUNCHES GOVERNMENT RELATIONS PROGRAM.” Business News For Home Medical Equipment Providers, 21 June 2023, www.hmenews.com/article/aeroflow-launches-government-relations-program.










