A sleep apnea tonsillectomy is a one-time surgical procedure that can help some sleep apnea patients avoid nightly CPAP treatments. As someone who suffers from obstructive sleep apnea (OSA), how do you know if removing the tonsils and/or adenoids is a sensible option for you? How might it alleviate OSA symptoms? And isn’t that a pediatric surgery? Stick with us as we dive into the details to help you determine if a tonsillectomy could be an option for you. It may be worth a conversation with your doctor or sleep specialist.
The Role Tonsils And Adenoids Play In Our Bodies
When considering this surgery, it helps to know what tonsils and adenoids do for your body. They are a part of the lymphatic system, which in turn is a part of your immune system. Tonsils and adenoids trap germs coming in through the mouth and nose. They also play a role in clearing infections.
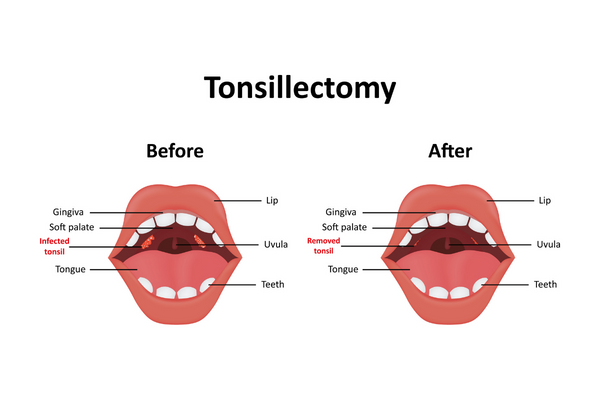
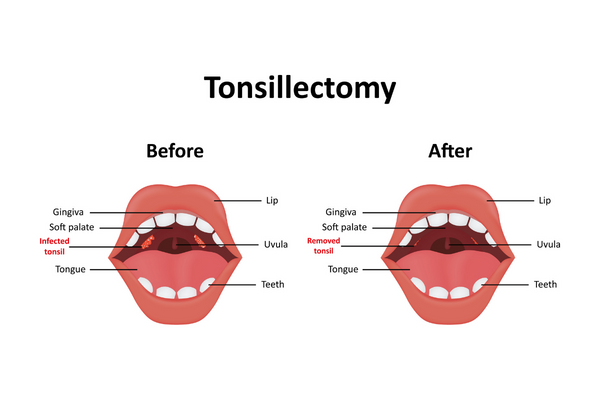
Removing your tonsils is called a tonsillectomy. Removing your adenoids is called an adenoidectomy. They are often removed together if the patient is young, which is called an adenotonsillectomy.
As adults, adenoids are typically not problematic. Tonsillectomies alone are more common for adults. Your doctor will help you decide if the loss of these lymphatic fixtures is worth the potential benefit to your OSA symptoms.
Tonsillectomy To Treat Sleep Apnea In Adults
It’s interesting why kids with sleep apnea often benefit from tonsillectomy in a way adults may not. It’s because their tonsils are naturally larger! Tonsils shrink with age. Plus, kids can’t generally tolerate CPAP therapy.
Tonsillar hypertrophy (enlarged tonsils) can be a naturally occurring anatomical feature, or the swelling can be due to recurrent tonsillitis. Either way, it’s worth asking your pediatrician about tonsil/adenoid removal if the OSA patient is young.
For adults, who have smaller tonsils and more coping skills, the first-line treatment for OSA is CPAP therapy - even for those with severe OSA. However, a tonsillectomy may be considered if an otolaryngologist (ear, nose, and throat doctor) determines an adult’s tonsils and/or adenoids are the cause of obstruction.
It’s important to know that a tonsillectomy is not a magic bullet for most adult sleep apnea patients. Many will not experience total symptom loss, but could still enjoy a reduction in symptoms. In this case, you may still need CPAP treatment to maintain healthy oxygen levels, decrease loud snoring, and improve sleep quality in order to reduce the hallmark daytime sleepiness of sleep apnoeas.
When Tonsillectomy Is Recommended For OSA
Sleep apnea tonsillectomy is more commonly recommended for young patients. Obesity in children is a well-documented issue, but obesity itself is not the only culprit behind sleep-disordered breathing in young patients. Obese and nonobese children alike suffer from sleep-disordered breathing due enlarged tonsil size.
If adult OSA patients have tried everything short of surgery (or have had a doctor confirm tonsillar obstruction) your healthcare provider may consider tonsillectomy. Without obstruction, you would typically attempt the following treatment options before opting for surgical tonsillectomy:
Alternative Surgical Treatments For Sleep Apnea
You and your doctor may begin a discussion about tonsillectomy only to decide that other surgical interventions are more appropriate for you. Some procedures involve adjusting the position of your jaw or reducing the volume of tissue in your upper airway, while others are designed to stimulate and tone your throat and neck muscles so they won’t be prone to collapse. Your overall health, weight, and the severity of your OSA will help determine the best choice for you.
What To Keep In Mind
Non-invasive measures are always preferred for adults. Luckily, there are a lot of lifestyle treatment options for sleep apnea that don’t involve going under the knife. There are also a lot of CPAP machine options and accessories to increase your comfort. It may take a while to get used to the equipment, but CPAP is the gold standard for non-invasive sleep apnea treatment.
Even if you do get a sleep apnea tonsillectomy, doctors typically recommend continuing your CPAP treatments postoperatively. This will continue until your doctor is satisfied that the tonsillectomy is healed and doing what you both hoped. Let your dedicated Aeroflow Sleep Specialist know that you've had any surgeries too, so they can stay abreast of your situation when recommending new or replacement CPAP supplies.
If you have not been diagnosed with sleep apnea, it’s important to be sure apnea sleep disorders are treated effectively. Untreated OSA can cause low oxygen levels and high blood pressure. This taxes the cardiovascular system and raises the patient’s risk of heart failure, regardless of your tonsil size.
Obstructive sleep apnea syndrome is a serious breathing disorder, so be sure to get to your follow-up appointments and keep in mind how your choices may affect your condition. For the sake of your health, it is critical to keep up your commitment to whatever treatment options you choose!
References
U.S. Department of Health and Human Services. (2019, March 5). Understanding recurrent tonsillitis. National Institutes of Health. Retrieved September 22, 2022, from https://www.nih.gov/news-events/nih-research-matters/understanding-recurrent-tonsillitis
Reckley LK, Fernandez-Salvador C, Camacho M. The effect of tonsillectomy on obstructive sleep apnea: an overview of systematic reviews. Nat Sci Sleep. 2018 Apr 4;10:105-110. doi: 10.2147/NSS.S127816. PMID: 29670412 ; PMCID: PMC5894651 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5894651/
Cherney, Kristeen. “Surgery For Sleep Apnea.” Edited by Fred Aleskerov, Healthline, Healthline, 1 July 2021, https://www.healthline.com/health/surgery-for-sleep-apnea.









