A 2021 study estimated that more than one in five adults in the United States deals with a mental illness. The connection between sleep and mental health is undeniable—poor sleep can contribute to mental health challenges, while mental health issues can disrupt sleep. We’ve teamed up with Dr. Chris Allen—a Board-Certified Sleep Medicine Physician, Pediatric Neurologist, and Aeroflow Sleep Science Advisor—to explore the effects of sleep on your mental health.
Can Sleep Deprivation Make You More Emotional?
A lack of sleep hurts your overall emotional well-being, just like sleeping well will allow you to live better. According to the National Sleep Foundation, “Good quality sleep can help you better regulate your emotions and improve your cognitive skills.” This is because our bodies and brains go through a restorative process that repairs the body’s cells when we sleep and helps us process our emotions and create memories.
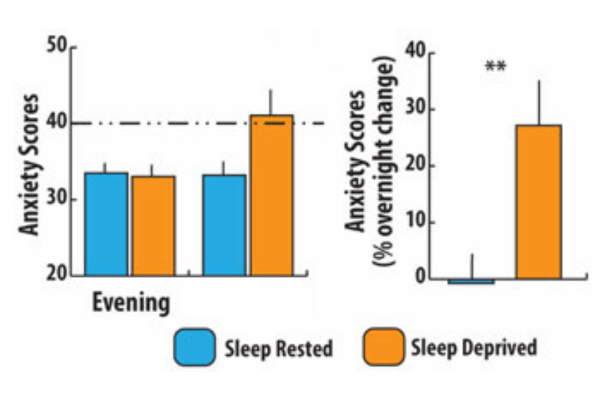
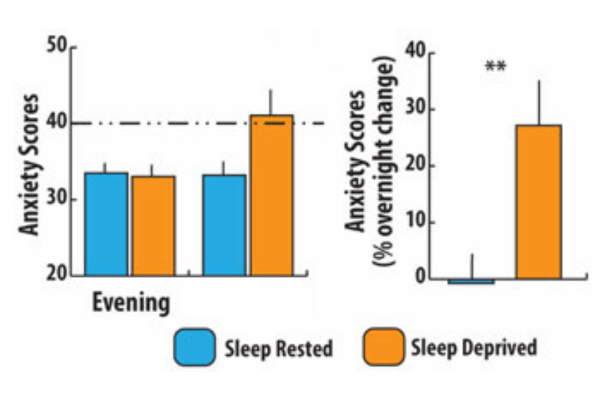
Conversely, poor sleep quality often makes it harder to regulate emotions. After a night of poor sleep, you may feel more irritable or struggle to cope with daily stressors. Dr. Allen shares, “There’s a high percentage of patients that have mental disorders; such as depression and anxiety.” This makes sense, as regular sleep problems often coincide with depressive symptoms and other mental health disorders.
How Are Your Sleep And Mental Health Connected?
“Quality sleep definitely plays a role in mental health,” Dr. Allen affirms. Sleep and mental health are tightly connected, with mental health issues also leading to sleep difficulties. For example, individuals with an anxiety disorder, post-traumatic stress disorder, or ADHD may struggle to go to sleep, stay asleep, and/or experience daytime sleepiness.
Meanwhile, individuals who have bipolar disorder may experience irregular sleep patterns, and individuals with schizophrenia may suffer from circadian rhythm disorders or chronic insomnia. The connection between sleep and mental health is evident, as these conditions can severely disrupt the natural sleep cycle.
Interventions like cognitive behavioral therapy (CBT) can help manage mental health disorders. Additionally, the Mayo Clinic reveals how CBT can benefit an individual’s sleep health. After all, some of the symptoms mentioned above—daytime sleepiness, irregular sleep patterns, and insomnia—can even point to obstructive sleep apnea (OSA.)
Does Improving Sleep Quality Benefit Anxiety & Depression?
Yes, effectively treating a sleep disorder leads to better sleep quality and mental health.
As we discussed earlier, poor sleep quality can lead to an increase in anxiety and depression levels, and it works the other way too. Improvements in sleep quality have a positive impact on mental health overall. In a recent study, researchers detail how enhancing sleep quality leads to decreased anxiety and depression levels, proving that a good night’s sleep is beneficial!
The same is true for individuals diagnosed with sleep disorders. Yet another study found that patients with sleep apnea and mental health issues often see reduced anxiety and depression symptoms once they’ve received treatment in the form of a CPAP machine.
How Much Sleep Is Needed For Your Mental Health?
You can improve your sleep quality by getting enough sleep for your mental health. The American Academy of Sleep Medicine (AASM) recommends that the average adult sleep seven or more hours per night regularly. While the amount of sleep your body needs can vary from person to person, it’s essential for your mental and physical health to get enough sleep, but one in three adults is not getting the recommended 7 hours.
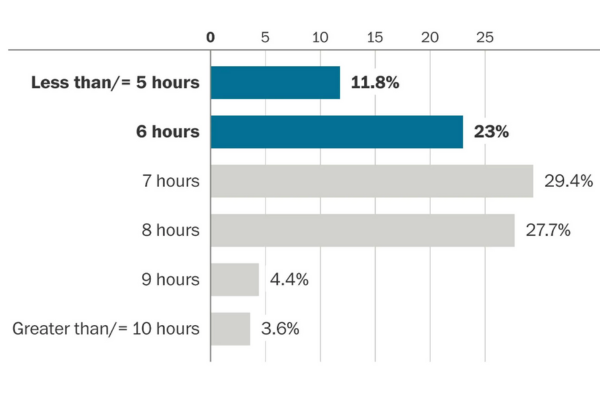
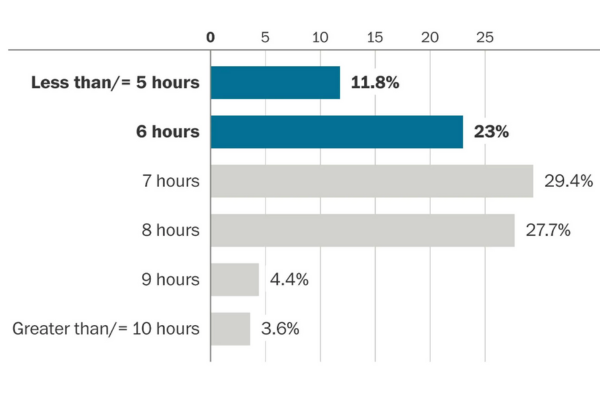
Sleeping less than 7 hours is associated with adverse health outcomes, such as depression, stroke, heart disease, obesity, and impaired immune function. Because sleeping less than 7 hours can negatively impact your brain and body, you should aim for at least 7 hours of sleep per night regardless of age, assigned sex at birth, and health conditions.
When Do Mental Health Problems Point To A Sleep Disorder?
Sleep disorders can exacerbate mental health problems. If you are experiencing challenges with your mental health and/or getting good quality sleep, reach out to your healthcare provider as soon as possible. This should also become a priority if any of the sleep apnea symptoms mentioned earlier currently affect your day-to-day life.
Get the Support You Need with Aeroflow Sleep
If you’ve already been diagnosed with sleep apnea, Aeroflow Sleep can help you get the CPAP supplies you need, covered up to 100% through insurance. Take 5 minutes to fill out our qualify form, so we can review your eligibility for the treatment you need to get a better quality of sleep.
References
“Mental Illness.” National Institute of Mental Health, U.S. Department of Health and Human Services, www.nimh.nih.gov/health/statistics/mental-illness. Accessed 3 May 2024.
“How Is Your Sleep Health Linked to Your Mental Health?” National Sleep Foundation, National Sleep Foundation, 8 Mar. 2023, www.thensf.org/how-is-your-sleep-health-linked-to-your-mental-health/.
“Insomnia Treatment: Cognitive Behavioral Therapy Instead of Sleeping Pills.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 5 Apr. 2023, www.mayoclinic.org/diseases-conditions/insomnia/in-depth/insomnia-treatment/art-20046677#:~:text=CBT%20can%20benefit%20nearly%20anyone,CBT%20has%20harmful%20side%20effects.
Wang, Yingting et al. “Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China's Xizang Region: The Mediating Effect of Cognitive Emotion Regulation.” Behavioral sciences (Basel, Switzerland) vol. 13,10 861. 20 Oct. 2023, doi:10.3390/bs13100861
Lee, Ming-Chung et al. “Effects of continuous positive airway pressure on anxiety, depression, and major cardiac and cerebro-vascular events in obstructive sleep apnea patients with and without coronary artery disease.” Ci ji yi xue za zhi = Tzu-chi medical journal vol. 29,4 (2017): 218-222. doi:10.4103/tcmj.tcmj_128_17
Watson, Nathaniel F et al. “Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society.” Sleep vol. 38,6 843-4. 1 Jun. 2015, doi:10.5665/sleep.4716











