Sleep apnea can be terrifying, both for the patient and their loved ones. You may wake up suddenly, gasping for air, and feeling like you’re choking or suffocating. Or you may witness your sleep partner stop breathing entirely while they sleep. But can you actually die from sleep apnea?
It may sound unbelievable, but Obstructive Sleep Apnea (OSA) is actually linked to an increase in the risk of death from all causes. That’s because the impacts of OSA can affect your body as well as your mental state. Below, we’ll explore what the science says about whether you can die from sleep apnea and, more importantly, how you can continue to live a long and healthy life.
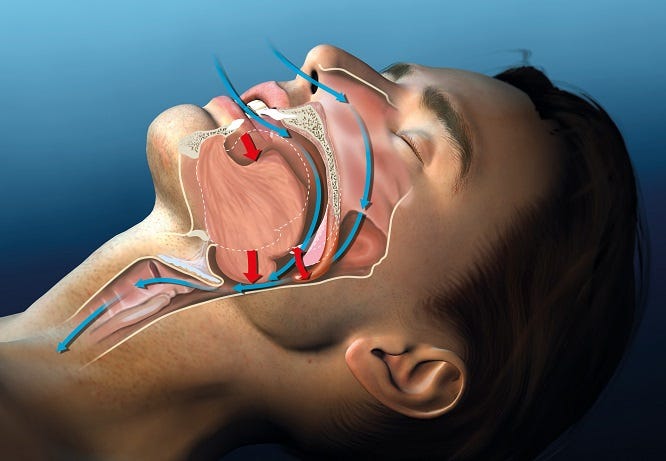
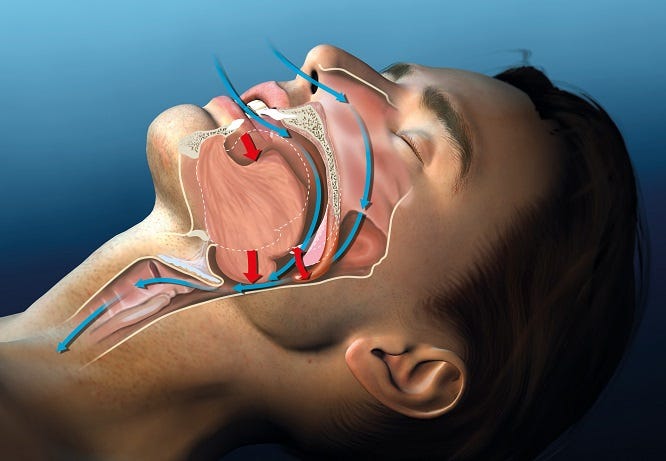
How Sleep Apnea Affects The Body
During an apnea or hypopnea event the muscles of your upper airways collapse, preventing you from getting enough air and dramatically reducing your blood oxygen levels.
Your body responds to this by releasing adrenaline and other stress hormones to try to force yourself to breathe again. These hormone levels are similar to a fight-or-flight response and can stay elevated for hours afterward, potentially causing:
- Increased heart rate
- High blood pressure
- Abnormal heart rhythms (atrial fibrillation)
- Narrowing of the arteries
In turn, these effects can contribute to or worsen health conditions such as hypertension and heart disease, and lead to an increased risk of heart attack and stroke.
In fact, according to Dr. Virend Somers, a cardiologist with the Mayo Clinic, “[...] if you have sleep apnea, your risk of sudden death increases almost twofold, particularly if you stopped breathing more than 20 times per hour of sleep and if you had severe falls in oxygen saturation during sleep.”
Apnea- Full stop in breathing for 10 seconds or greater.
Hypopnea- Reduction in breathing for 10 seconds or greater.
Apnea-Hypopnea Index (AHI)- The severity of sleep apnea measured in the number of apneas or hypopneas per hour of sleep.
Can You Die From Sleep Apnea?
A common question from sleep apnea patients is whether OSA can cause you to suffocate in your sleep. This is a different question from whether you can die from sleep apnea.
While apnea events do cause you to stop breathing, they also cause you to awaken, so you’re extremely unlikely to suffocate from OSA by itself. However, while you’re unlikely to die from an apnea event directly, untreated sleep apnea is directly tied to an increased risk of premature death.
Take a look at what the research shows:
- Severe sleep apnea predicts an 81% increase in the risk of sudden cardiac death.
“Our analysis showed that for the lowest [nighttime oxygen levels], the best discriminating threshold of 78% predicts an 81% increase in the risk of [sudden cardiac death].”
https://www.sciencedirect.com/science/article/pii/S0735109713022511 - Sleep apnea increases risk of heart attack and death by 30% over 4-5 years.
“The nighttime breathing disorder known as sleep apnea increases a person’s risk of having a heart attack or of dying by 30 percent over a period of four to five years, according to a Yale School of Medicine study.”
https://news.yale.edu/2007/05/24/sleep-apnea-increases-risk-heart-attack-and-diabetes - Your risk of stroke increases as your AHI goes up.
“The risk of stroke increased 6% with every unit increase in baseline [Apnea-Hypopnea Index] from 5 to 25.”
https://www.atsjournals.org/doi/full/10.1164/rccm.200911-1746OC - Sleep apnea is often found in patients with heart failure.
“Studies of consecutive patients with heart failure (HF) have consistently described that sleep apnea (SA) is a highly prevalent comorbid condition present in approximately 40 to 60% of subjects, a rate far higher than in the general population.”
https://www.atsjournals.org/doi/full/10.1164/rccm.201003-0406OC - Severe sleep apnea makes you 3 times more likely to die from all causes.
“Mortality follow-up of the Wisconsin Sleep Cohort [...] indicates that severe [sleep disordered breathing] is significantly associated with a 3-fold increased all-cause mortality risk [...] independently of age, sex, BMI, and other potential confounders.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2542952/
What Does Sleep Apnea Feel Like?


Mild Sleep Apnea (5-15 AHI)
The American Sleep Apnea Association defines mild sleep apnea as having an average of 5 to 15 pauses in breathing while asleep. These pauses may not be as regular as they are in the GIF, but imagine how it would feel spread out across an entire night.
Moderate Sleep Apnea (15-30 AHI)
Moderate sleep apnea involves 15 to 30 events of stopped or reduced breathing for 10 seconds or longer each time. If you made it through the full minute, you can probably imagine why OSA patients suffer from headaches, irritability, and difficulty concentrating.


Severe Sleep Apnea (30+ AHI)
Severe sleep apnea starts at 30 obstructions per hour, but has been known to be as high as over 100 events per hour! Breathing along with the GIF was probably pretty uncomfortable, so you may have some understanding of how OSA can impact medical conditions like cardiovascular disease.
Sleep apnea can be hard to recognize since, by definition, it happens when you’re asleep. Most apnea patients begin to suspect something is wrong when they notice the daytime symptoms of sleep apnea– these include daytime sleepiness, daytime fatigue or weakness, mood changes, memory problems, or frequently waking to a headache, dry mouth, or sore throat.
While you won’t recognize the feeling of an apnea event when it happens, we’ve created a series of GIFs that help simulate the feeling of sleep apnea. They’re designed to give you an idea of just how serious OSA can be.
Try to breathe along with the pattern shown for one minute:
Can You Live a Long Life with Sleep Apnea?
The good news is that there is an easy and non-invasive way to protect your health! Just as untreated sleep apnea increases the risk of death, a CPAP machine can virtually eliminate that higher risk.
“Use of the continuous positive airway pressure (CPAP) mask was tied to a 62% decline in the odds for death over 11 years of follow-up.”
https://www.webmd.com/sleep-disorders/sleep-apnea/news/20190415/cpap-brings-longer-life-for-those-with-sleep-apnea
CPAP therapy is considered front-line sleep medicine for the treatment of Obstructive Sleep Apnea, because it is the most effective nonsurgical option. CPAP use has been shown to lower blood pressure and reduce the risk of cardiac arrest and other health problems, especially in those with moderate to severe sleep apnea.
With CPAP therapy it is possible to live a long and healthy life!
What Do I Do If I Think I May Have Sleep Apnea?
There are certain risk factors that make you more likely to have sleep apnea. These include loud snoring, obesity, being male or assigned male at birth, having a large neck, and a family history of OSA. However, it is possible to have sleep apnea even if you don’t match any of these descriptions.
The only way to know for sure is to have an exam called a sleep study. A sleep study can be performed in-lab or at-home, but either way you’ll need to have a prescription. So, if you or your partner suspect that you may have sleep apnea you should talk to your doctor right away.
If your sleep study determines that you have Obstructive Sleep Apnea, your doctor will most likely prescribe CPAP therapy. That’s where Aeroflow Sleep comes in! We’ll match you with a Sleep Specialist who will work with your doctor and insurance provider to simplify the process of getting a CPAP.
Your personal Sleep Specialist can help you choose the machine that’s right for you, then handle all of the paperwork for you! All you need to do is fill out our simple qualify form, and we’ll take it from there.
With such an easy solution, there’s no reason to accept the risks that sleep apnea causes. If you think you may have sleep apnea, you owe it to yourself and your loved ones to talk to your doctor about it today. Then talk to Aeroflow Sleep!
References
- https://newsnetwork.mayoclinic.org/discussion/obstructive-sleep-apnea-raises-risk-of-sudden-cardiac-death-mayo-clinic-finds/
- https://news.yale.edu/2007/05/24/sleep-apnea-increases-risk-heart-attack-and-diabetes
- https://www.atsjournals.org/doi/full/10.1164/rccm.200911-1746OC
- https://www.atsjournals.org/doi/full/10.1164/rccm.201003-0406OC
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2542952/
- https://www.sleepapnea.org/what-does-ahi-represent/
- https://www.webmd.com/sleep-disorders/sleep-apnea/news/20190415/cpap-brings-longer-life-for-those-with-sleep-apnea